ARTICLE
There has recently been a lot of discussion on social media regarding the capsule that forms around breast implants and how it should be treated. I am often asked by other surgeons what advice I give my patients. They say that they feel pressured to do a total capsulectomy when they know it may not be safe, or even possible. Is the capsule the cause of a woman’s symptoms and what happens if it is not totally removed?
What is the capsule?
The capsule does not refer to the outer wall of the breast implant. It is your own tissue and refers to the multiple layers of collagen manufactured by your body to contain the implant. It is Nature’s way of separating and excluding the implant (which it recognises as foreign) from the body. A capsule forms around all implants, including chin implants, cheek implants cardiac pacemakers etc. For a breast implant, it acts as a type of “bra” providing support for the implant and holding it in place. In some situations (for example when using an implant for post mastectomy reconstruction) some surgeons even add to the capsule by inserting a strip of artificial collagen (acellular dermal matrix or ADM) to provide extra support for the implant. If your implant were to leak silicone, the capsule will act as a barrier to prevent or delay the silicone from spreading into surrounding tissues. In this situation, the capsule is your protector and your friend.

What are the different types of capsule?
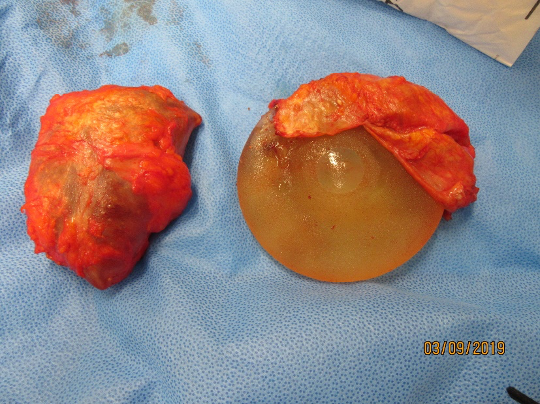
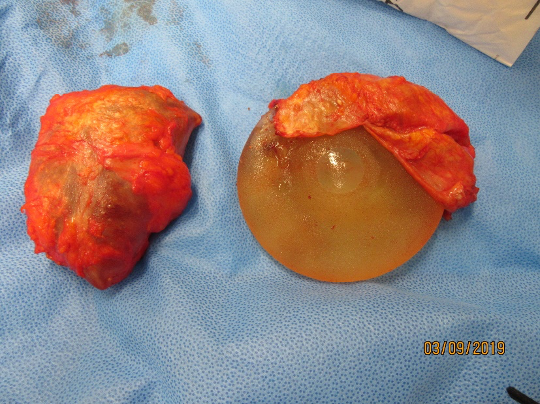
Capsules can be thin or thick. They can be multi layered. Sometimes a double capsule forms, with one capsule tightly adherent to the implant which is then surrounded by a second capsule. As a general rule, capsules that form around implants that have been placed under the muscle tend to be only a thin layer of collagen which is very adherent to the surrounding tissues, while those capsules forming around implants placed in front of the muscle tend to be much thicker and less adherent.
The capsule that the body forms varies according to the surface texture of the implant. Smooth-walled implants placed under the muscle produce the thinnest capsules. Macro textured implants tend to produce much thicker capsules and occasionally a double capsule forms as described above.
When one examines the capsule under the microscope one sees multiple layers of collagen. Occasionally however (especially around textured breast implants) a number of inflammatory cells are seen indicating chronic inflammation. These are the patients that tend to develop the symptoms of Breast Implant Associated Illness (BIAI).

What is Breast Implant Associated Illness (BIAI)?
Breast Implant Associated Illness refers to recurrent and persistent flu like symptoms that develop in women with breast implants, especially textured breast implants. Symptoms commonly reported are fatigue, anxiety, foggy thinking, memory loss, headaches, muscle pains and even hair loss and skin rashes. Given that the total surface area of two breast implants is at least 6% of the body surface area, having chronic inflammation of such an extent (the equivalent of a burn of almost one arm!) it is understandable that women who have this degree of inflammation around their breast implants (especially if they are textured with an even larger surface area) should feel unwell. Fortunately, once the implants are removed, there is no further stimulus for inflammation. The inflammation then disappears leaving only the collagen of the capsule. The symptoms of BIAI then settle over a few weeks whether or not all the capsule has been removed.
How should the capsule be treated?
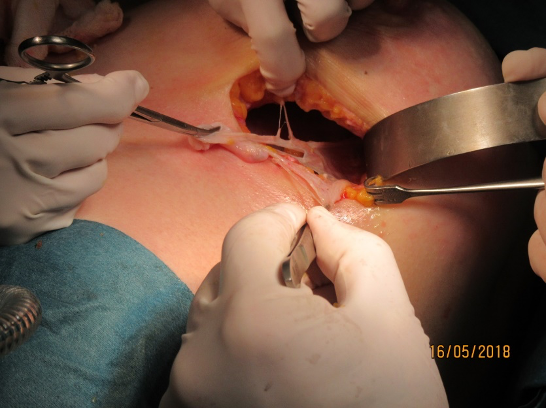
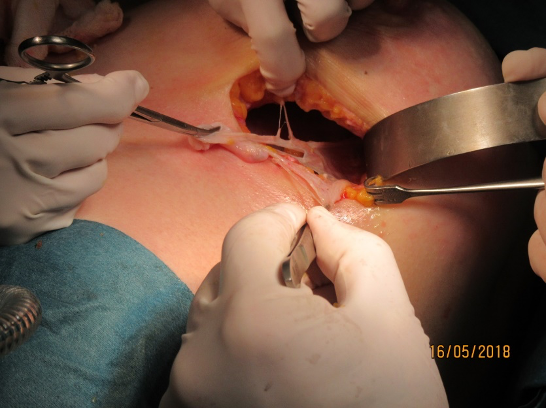
With so many different types of capsules (thick, thin, double, calcified, in front of the muscle, behind the muscle) it is obvious that every case is different. Sometimes, attempting to remove the capsule can be really dangerous. Especially when the implant has been placed under the muscle when the posterior part of the capsule is adherent to the rib cage and thin intercostal muscles. Attempting removal can result in a pneumothorax (collapsed lung). This can be a life threatening event. With implants that are over 20 years old and have been placed in front of the muscle, sometimes we find that the capsule is extremely thick and heavily calcified. In these instances an en-bloc or total capsulectomy is relatively easy. It is this type of case that is often shown on the Internet as a demonstration of en-bloc capsulectomy. Even in these situations however, it is possible for considerable damage to be done to the underlying muscle and the surrounding breast tissue, such that considerable deformity can be produced. Indeed one of the common applications of fat transfer is correction of deformities caused by total capsulectomy.
So what should I do?
Given the complexity of this situation it is important that you consult a surgeon who is experienced in this procedure and is able to give you appropriate and personalised advice. The advice may be that you require an En-bloc or total capsulectomy – especially if your implants are very old and the capsule is in front of the muscle, thick and calcified. It may even be your preference to have this type of procedure. However the surgeon’s first responsibility is to you and your safety. No surgeon should feel under pressure to persist in an attempt to remove a capsule when severe bleeding, tissue damage or pneumothorax is a likely outcome. Remember that the capsule is your own tissue and not foreign. If your symptoms are due to inflammation of the capsule, this will subside once the implants are removed and you will recover -even if the capsule could not been completely removed.
Allan Kalus
ARTICLE
Understanding the Capsule that forms around Breast Implants
There has recently been a lot of discussion on social media regarding the capsule that forms around breast implants and how it should be treated. I am often asked by other surgeons what advice I give my patients. They say that they feel pressured to do a total capsulectomy when they know it may not be safe, or even possible. Is the capsule the cause of a woman’s symptoms and what happens if it is not totally removed?
What is the capsule?
The capsule does not refer to the outer wall of the breast implant. It is your own tissue and refers to the multiple layers of collagen manufactured by your body to contain the implant. It is Nature’s way of separating and excluding the implant (which it recognises as foreign) from the body. A capsule forms around all implants, including chin implants, cheek implants cardiac pacemakers etc. For a breast implant, it acts as a type of “bra” providing support for the implant and holding it in place. In some situations (for example when using an implant for post mastectomy reconstruction) some surgeons even add to the capsule by inserting a strip of artificial collagen (acellular dermal matrix or ADM) to provide extra support for the implant. If your implant were to leak silicone, the capsule will act as a barrier to prevent or delay the silicone from spreading into surrounding tissues. In this situation, the capsule is your protector and your friend.

What are the different types of capsule?
Capsules can be thin or thick. They can be multi layered. Sometimes a double capsule forms, with one capsule tightly adherent to the implant which is then surrounded by a second capsule. As a general rule, capsules that form around implants that have been placed under the muscle tend to be only a thin layer of collagen which is very adherent to the surrounding tissues, while those capsules forming around implants placed in front of the muscle tend to be much thicker and less adherent.
The capsule that the body forms varies according to the surface texture of the implant. Smooth-walled implants placed under the muscle produce the thinnest capsules. Macro textured implants tend to produce much thicker capsules and occasionally a double capsule forms as described above.
When one examines the capsule under the microscope one sees multiple layers of collagen. Occasionally however (especially around textured breast implants) a number of inflammatory cells are seen indicating chronic inflammation. These are the patients that tend to develop the symptoms of Breast Implant Associated Illness (BIAI).

What is Breast Implant Associated Illness (BIAI)?
Breast Implant Associated Illness refers to recurrent and persistent flu like symptoms that develop in women with breast implants, especially textured breast implants. Symptoms commonly reported are fatigue, anxiety, foggy thinking, memory loss, headaches, muscle pains and even hair loss and skin rashes. Given that the total surface area of two breast implants is at least 6% of the body surface area, having chronic inflammation of such an extent (the equivalent of a burn of almost one arm!) it is understandable that women who have this degree of inflammation around their breast implants (especially if they are textured with an even larger surface area) should feel unwell. Fortunately, once the implants are removed, there is no further stimulus for inflammation. The inflammation then disappears leaving only the collagen of the capsule. The symptoms of BIAI then settle over a few weeks whether or not all the capsule has been removed.
How should the capsule be treated?
With so many different types of capsules (thick, thin, double, calcified, in front of the muscle, behind the muscle) it is obvious that every case is different. Sometimes, attempting to remove the capsule can be really dangerous. Especially when the implant has been placed under the muscle when the posterior part of the capsule is adherent to the rib cage and thin intercostal muscles. Attempting removal can result in a pneumothorax (collapsed lung). This can be a life threatening event. With implants that are over 20 years old and have been placed in front of the muscle, sometimes we find that the capsule is extremely thick and heavily calcified. In these instances an en-bloc or total capsulectomy is relatively easy. It is this type of case that is often shown on the Internet as a demonstration of en-bloc capsulectomy. Even in these situations however, it is possible for considerable damage to be done to the underlying muscle and the surrounding breast tissue, such that considerable deformity can be produced. Indeed one of the common applications of fat transfer is correction of deformities caused by total capsulectomy.
So what should I do?
Given the complexity of this situation it is important that you consult a surgeon who is experienced in this procedure and is able to give you appropriate and personalised advice. The advice may be that you require an En-bloc or total capsulectomy – especially if your implants are very old and the capsule is in front of the muscle, thick and calcified. It may even be your preference to have this type of procedure. However the surgeon’s first responsibility is to you and your safety. No surgeon should feel under pressure to persist in an attempt to remove a capsule when severe bleeding, tissue damage or pneumothorax is a likely outcome. Remember that the capsule is your own tissue and not foreign. If your symptoms are due to inflammation of the capsule, this will subside once the implants are removed and you will recover -even if the capsule could not been completely removed.
Allan Kalus